Esomeprazole (Monograph)
Brand names: NexIUM, Vimovo (combination)
Drug class: Proton-pump Inhibitors
VA class: GA900
Chemical name: 5-Methoxy-2-[(S)[(4-methoxy-3,5-dimethyl-2-pyridinyl)methyl]sulfinyl]-1H-benzimidazole magnesium salt trihydrate
Molecular formula: C34H36MgN6O6S2•3H2OC17H18N3O3S•Na
CAS number: 217087-09-7
Introduction
Acid- or proton-pump inhibitor; gastric antisecretory agent. S-isomer of omeprazole.
Uses for Esomeprazole
Gastroesophageal Reflux (GERD)
Short-term treatment of symptomatic GERD (e.g., heartburn) in patients without erosive esophagitis.
Short-term treatment of erosive esophagitis (diagnostically confirmed) in patients with GERD. Short-term treatment of erosive esophagitis due to acid-mediated GERD in infants.
Maintain healing, symptom resolution, and decrease recurrence of erosive esophagitis.
IV as short-term alternative to oral therapy in patients with erosive esophagitis who are unable to take the drug orally; safety and efficacy not established beyond 10 days.
Duodenal Ulcer
Treatment of Helicobacter pylori infection and duodenal ulcer disease (active duodenal ulcer or history of duodenal ulcer in the past 5 years). Used in conjunction with amoxicillin and clarithromycin (triple therapy).
NSAIA-associated Ulcers
Reduction in the occurrence of gastric ulcers associated with chronic NSAIA therapy in patients at risk (i.e., ≥60 years of age and/or history of gastric ulcer). Effect on occurrence of duodenal ulcers not established.
Crohn’s Disease-associated Ulcers
Some evidence for use of proton-pump inhibitors (e.g., omeprazole) for gastric acid suppressive therapy as an adjunct in the management of upper GI Crohn’s disease† [off-label], including esophageal, gastroduodenal, and jejunoileal disease.
Esomeprazole Dosage and Administration
Administration
Administer orally or IV.
Oral Administration
Administer esomeprazole capsules and oral suspension orally at least 1 hour before a meal. Administer esomeprazole/naproxen fixed-combination tablets at least 30 minutes before a meal. (See Food under Pharmacokinetics.)
Antacids may be used concomitantly as needed for pain relief.
Capsules
Swallow capsules intact; do not chew or crush.
Alternatively, open capsule and mix contents with 1 tablespoon applesauce; swallow immediately without chewing. Applesauce should not be hot and should be soft enough to swallow without chewing.
Powder for Oral Suspension
Mix contents of 2.5- or 5-mg packet with 5 mL of water.
Mix contents of 10-, 20-, or 40-mg packet with 15 mL of water.
If a single dose requires 2 packets, reconstitute oral suspension with twice the water needed for 1 packet.
After mixing suspension with appropriate amount of water, allow mixture to thicken for 2–3 minutes. Stir mixture and consume within 30 minutes of preparation. If any drug mixture remains in container after ingestion, mix with additional water and ingest immediately.
NG Tube
May administer suspension prepared from opened capsules through NG tube; may administer suspension prepared from powder for oral suspension through NG tube or gastric tube (6 French or larger).
Capsules: Open capsule, empty intact granules into 60-mL catheter-tipped syringe, and mix with 50 mL of water. Replace plunger and shake well for 15 seconds. Hold syringe with tip upright and check tip for remaining granules. Administer immediately through NG tube; flush with additional water. Do not administer if pellets have dissolved or disintegrated.
Powder for oral suspension: Mix contents of 2.5- or 5-mg packet with 5 mL of water and contents of 10-, 20-, or 40-mg packet with 15 mL of water in a catheter-tipped syringe; shake immediately, then allow mixture to thicken for 2–3 minutes. Shake syringe and administer through NG or gastric tube (6 French or larger) within 30 minutes of preparation. Refill syringe with additional water (5 or 15 mL, respectively) and flush NG or gastric tube.
Esomeprazole/Naproxen Fixed-combination Tablets
Swallow tablets whole with liquid; do not split, chew, crush, or dissolve tablets.
IV Administration
For solution compatibility information, see Compatibility under Stability.
Administer by slow direct IV injection or by IV infusion.
Flush the IV line with 0.9% sodium chloride, lactated Ringer’s, or 5% dextrose injection before and after administration.
Do not administer with any other drugs or diluents because of potential incompatibilities.
Reconstitution
For direct IV injection in adults, reconstitute vial containing 20 or 40 mg of esomeprazole with 5 mL of 0.9% sodium chloride injection.
For IV infusion in adults, reconstitute vial containing 20 or 40 mg of esomeprazole with 5 mL of 5% dextrose, 0.9% sodium chloride, or lactated Ringer’s injection. Dilute reconstituted solution prior to infusion.
For IV infusion in pediatric patients 1 month to 17 years of age, reconstitute vial containing 20 or 40 mg of esomeprazole with 5 mL of 0.9% sodium chloride injection to provide a solution containing 4 or 8 mg/mL, respectively. Dilute reconstituted solution prior to infusion.
Dilution
For IV infusion in adults, dilute the reconstituted solution to a final volume of 50 mL with a compatible IV solution (see Compatibility under Stability).
For IV infusion in pediatric patients 1 month to 17 years of age, dilute the reconstituted 4- or 8-mg/mL solution to a final volume of 50 mL with 0.9% sodium chloride injection to yield a final concentration of 0.4 or 0.8 mg/mL, respectively. Withdraw the appropriate dose from the diluted solution.
Rate of Administration
IV injection in adults: Administer reconstituted solution by slow (over ≥3 minutes) direct IV injection.
IV infusion in adults and pediatric patients: Administer diluted solution by IV infusion over 10–30 minutes.
Dosage
Available as esomeprazole magnesium and esomeprazole sodium; dosage expressed in terms of esomeprazole.
Pediatric Patients
GERD
GERD Without Erosive Esophagitis
OralChildren 1–11 years of age: 10 mg once daily for up to 8 weeks.
Adolescents 12–17 years of age: 20 or 40 mg once daily for up to 8 weeks.
Treatment of Erosive Esophagitis
Oral|
Age |
Body Weight |
Esomeprazole Dosage |
|---|---|---|
|
1 month to <1 year of age |
3–5 kg |
2.5 mg once daily for up to 6 weeks |
|
>5 to 7.5 kg |
5 mg once daily for up to 6 weeks |
|
|
>7.5 to 12 kg |
10 mg once daily for up to 6 weeks |
|
|
1–11 years of age |
<20 kg |
10 mg once daily for up to 8 weeks |
|
≥20 kg |
10 or 20 mg once daily for up to 8 weeks |
Infants 1 month to <1 year of age: 0.5 mg/kg once daily.
Children and adolescents 1–17 years of age: 10 mg once daily in those weighing <55 kg; 20 mg once daily in those weighing ≥55 kg.
Discontinue IV administration as soon as patient can take the drug orally.
Adults
GERD
GERD Without Erosive Esophagitis
Oral20 mg once daily for 4 weeks; may give an additional 4 weeks of therapy. Chronic proton-pump inhibitor therapy may be appropriate.
Treatment of Erosive Esophagitis
Oral20 or 40 mg once daily for 4–8 weeks; may give an additional 4–8 weeks of therapy.
IV20 or 40 mg once daily. Safety and efficacy not established beyond 10 days; discontinue IV administration as soon as patient can take the drug orally.
Maintenance of Healing of Erosive Esophagitis
Oral20 mg once daily; not studied >6 months.
Duodenal Ulcer
Helicobacter pylori Infection and Duodenal Ulcer
OralTriple therapy: 40 mg once daily for 10 days in conjunction with amoxicillin and clarithromycin.
NSAIA-associated Ulcers
Prevention of Gastric Ulcers
Oral20 or 40 mg once daily; not studied >6 months.
Esomeprazole/naproxen fixed combination: Esomeprazole 20 mg (with naproxen 375 or 500 mg) twice daily. Do not use fixed combination if esomeprazole dosage requirement is <40 mg daily.
Prescribing Limits
Pediatric Patients
GERD
GERD Without Erosive Esophagitis
OralChildren 1–11 years of age: Dosages >1 mg/kg daily not studied.
Treatment of Erosive Esophagitis
OralInfants 1 month to <1 year of age: Dosages >1.33 mg/kg daily not studied.
Children 1–11 years of age: Dosages >1 mg/kg daily not studied.
Special Populations
Hepatic Impairment
Oral or IV dosage should not exceed 20 mg once daily in patients with severe (Child-Pugh class C) hepatic impairment. No dosage adjustment required for mild or moderate (Child-Pugh class A or B, respectively) hepatic impairment.
Esomeprazole/naproxen fixed combination not recommended in patients with severe hepatic impairment.
Renal Impairment
Esomeprazole/naproxen fixed combination not recommended in patients with Clcr <30 mL/minute.
Cautions for Esomeprazole
Contraindications
-
Known hypersensitivity to esomeprazole, any ingredient in the formulation, or other substituted benzimidazoles (e.g., lansoprazole, omeprazole, pantoprazole, rabeprazole).
Warnings/Precautions
Sensitivity Reactions
Hypersensitivity Reactions
Hypersensitivity reactions (e.g., angioedema, anaphylactic shock) reported.
Gastric Malignancy
Response to esomeprazole does not preclude presence of occult gastric neoplasm.
Atrophic Gastritis
Atrophic gastritis reported occasionally with long-term omeprazole use.
Clostridium difficile Infection
Proton-pump inhibitors associated with possible increased (1.4–2.75 times) risk of Clostridium difficile infection, including C. difficile-associated diarrhea and colitis (CDAD; also known as antibiotic-associated diarrhea and colitis or pseudomembranous colitis). Many patients also had other risk factors for CDAD. May be severe; colectomy and, rarely, death reported.
Use the lowest effective dosage and shortest duration of therapy appropriate for the patient's clinical condition.
Consider CDAD if persistent diarrhea develops and manage accordingly; initiate supportive therapy (e.g., fluid and electrolyte management), anti-infective therapy directed against C. difficile (e.g., metronidazole, vancomycin), and surgical evaluation as clinically indicated.
Bone Fracture
Several observational studies suggest that use of proton-pump inhibitors, particularly in high dosages (i.e., multiple daily doses) and/or for prolonged periods of time (i.e., ≥1 year), may be associated with increased risk of osteoporosis-related fractures of the hip, wrist, or spine. Magnitude of risk is unclear; causality not established. FDA is continuing to evaluate this safety concern.
Use the lowest effective dosage and shortest duration of therapy appropriate for the patient’s clinical condition.
Individuals at risk for osteoporosis-related fractures should receive an adequate intake of calcium and vitamin D; assess and manage these patients’ bone health according to current standards of care.
Hypomagnesemia
Hypomagnesemia, symptomatic and asymptomatic, reported rarely in patients receiving long-term therapy (≥3 months or, in most cases, >1 year) with proton-pump inhibitors, including esomeprazole. Serious adverse effects include tetany, seizures, tremors, carpopedal spasm, arrhythmias (e.g., atrial fibrillation, supraventricular tachycardia), and abnormal QT interval. Paresthesia, muscle weakness, muscle cramps, lethargy, fatigue, and unsteadiness may occur. Most patients required magnesium replacement and discontinuance of the proton-pump inhibitor. Hypomagnesemia resolved within 1 week (median) following discontinuance and recurred within 2 weeks (median) of rechallenge.
In patients expected to receive long-term proton-pump inhibitor therapy or in patients currently receiving digoxin or drugs that may cause hypomagnesemia (e.g., diuretics), consider measuring serum magnesium concentrations prior to initiation of prescription proton-pump inhibitor therapy and periodically thereafter.
Cardiovascular Effects
Preliminary safety data from 2 long-term clinical trials comparing esomeprazole or omeprazole with antireflux surgery in patients with severe GERD raised concerns about a potential increased risk of cardiac events (e.g., MI, heart failure, sudden death) in patients receiving these drugs. After reviewing data from these and other studies, FDA has concluded that long-term use of these drugs is not likely to be associated with an increased risk of such cardiac events. FDA recommends that clinicians continue to prescribe and patients continue to use these drugs in the manner described in the manufacturers’ labelings.
Respiratory Effects
Administration of proton-pump inhibitors has been associated with an increased risk for developing certain infections (e.g., community-acquired pneumonia).
Use of Fixed Combinations
When used in fixed combination with naproxen, consider the cautions, precautions, and contraindications associated with naproxen.
Specific Populations
Pregnancy
Category B.
Lactation
Not known whether esomeprazole is distributed into milk, but omeprazole is distributed into milk. Discontinue nursing or the drug.
Pediatric Use
Safety and efficacy of oral esomeprazole for short-term (4–8 weeks) treatment of GERD established in pediatric patients 1–17 years of age. Adverse effects and pharmacokinetics in children and adolescents similar to those reported in adults.
Safety and efficacy of oral esomeprazole for short-term (up to 6 weeks) treatment of erosive esophagitis due to acid-mediated GERD established in infants 1 month to <1 year of age. Oral esomeprazole was not more effective than placebo in a randomized, controlled, treatment-withdrawal study in infants 1–11 months of age with symptomatic GERD. Common adverse effects include irritability and vomiting.
Efficacy of oral esomeprazole not established in infants <1 month of age.
Safety and efficacy of IV esomeprazole for short-term treatment of GERD with erosive esophagitis established in pediatric patients 1 month to 17 years of age. Adverse effects consistent with the drug's known safety profile.
Safety and efficacy of IV esomeprazole in neonates <1 month of age not established.
Geriatric Use
No substantial differences in safety and efficacy relative to younger adults, but increased sensitivity cannot be ruled out.
Hepatic Impairment
Use with caution in patients with severe hepatic impairment. (See Hepatic Impairment under Dosage and Administration.)
Common Adverse Effects
Oral: Headache, diarrhea, nausea, flatulence, abdominal pain, constipation, dry mouth.
IV: Similar adverse effects as oral esomeprazole; also injection site reaction, dizziness/vertigo, pruritus.
Drug Interactions
Extensively metabolized by CYP isoenzymes, principally CYP2C19; also to lesser extent by CYP3A4. May inhibit CYP2C19; unlikely to inhibit CYP3A4, 1A2, 2A6, 2C9, 2D6, or 2E1.
Drugs Metabolized by Hepatic Microsomal Enzymes
Potential to inhibit metabolism of drugs metabolized by CYP2C19. Interaction unlikely with drugs metabolized by other CYP isoenzymes.
Drugs Affecting Hepatic Microsomal Enzymes
Combined inhibitors of CYP2C19 and CYP3A4: Potential pharmacokinetic interaction (increased esomeprazole exposure); esomeprazole dosage adjustment usually not required but may be considered in patients receiving high dosages (up to 240 mg daily), such as those with Zollinger-Ellison syndrome.
Inducers of CYP2C19 and/or CYP3A4: Potential pharmacokinetic interaction (decreased esomeprazole concentrations).
Drugs that Cause Hypomagnesemia
Potential pharmacologic interaction (possible increased risk of hypomagnesemia). Consider monitoring magnesium concentrations prior to initiation of prescription proton-pump inhibitor therapy and periodically thereafter. (See Hypomagnesemia under Cautions.)
Specific Drugs and Laboratory Tests
|
Drug or Test |
Interaction |
Comments |
|---|---|---|
|
Amoxicillin |
Pharmacokinetic interaction unlikely |
|
|
Atazanavir |
Possible altered oral absorption of atazanavir, resulting in decreased plasma atazanavir concentrations; possible loss of virologic response and development of drug resistance |
Manufacturer of esomeprazole states that concomitant administration with atazanavir is not recommended Antiretroviral treatment-naive patients: If a proton-pump inhibitor is used concomitantly with atazanavir, administer ritonavir-boosted atazanavir (atazanavir 300 mg and ritonavir 100 mg once daily with food); administer the proton-pump inhibitor approximately 12 hours before ritonavir-boosted atazanavir For treatment-naive patients, dosage of proton-pump inhibitor should not exceed omeprazole 20 mg daily (or equivalent) Antiretroviral treatment-experienced patients: Concomitant use of proton-pump inhibitors with atazanavir not recommended |
|
Cilostazol |
Possible increased concentrations of cilostazol and its active metabolite |
Consider reducing cilostazol dosage (from 100 mg twice daily to 50 mg twice daily) |
|
Clarithromycin |
Increased plasma concentrations of esomeprazole and 14-hydroxyclarithromycin |
Not considered clinically important |
|
Clopidogrel |
Esomeprazole (or omeprazole) reduces exposure to clopidogrel's active metabolite and decreases platelet inhibitory effects; additional data needed to fully elucidate potential clinical consequences (e.g., increased cardiovascular events) Dexlansoprazole, lansoprazole, or pantoprazole had less effect on clopidogrel's antiplatelet activity than did omeprazole or esomeprazole |
Avoid concomitant use of esomeprazole (or omeprazole) and clopidogrel Assess risks and benefits of concomitant proton-pump inhibitor and clopidogrel use in individual patients American College of Cardiology Foundation/American College of Gastroenterology/American Heart Association (ACCF/ACG/AHA) states that GI bleeding risk reduction with concomitant proton-pump inhibitor in patients with risk factors for GI bleeding (e.g., advanced age; concomitant use of warfarin, corticosteroids, or NSAIAs; H. pylori infection) may outweigh potential reduction in cardiovascular efficacy of antiplatelet treatment associated with a drug-drug interaction. In patients without such risk factors, ACCF/ACG/AHA states that risk/benefit balance may favor use of antiplatelet therapy without a proton-pump inhibitor. If concomitant therapy with a proton-pump inhibitor and clopidogrel is deemed necessary, consider using an agent with little or no CYP2C19-inhibitory activity; alternatively, consider using a histamine H2-receptor antagonist (ranitidine, famotidine, nizatidine) but not cimetidine (also a potent CYP2C19 inhibitor) |
|
Diazepam |
Decreased diazepam metabolism and increased plasma concentrations |
Not considered clinically important |
|
Digoxin |
Hypomagnesemia (e.g., resulting from long-term use of proton-pump inhibitors) sensitizes the myocardium to digoxin and, thus, may increase risk of digoxin-induced cardiotoxic effects See table entry for gastric pH-dependent drugs |
Consider monitoring magnesium concentrations prior to initiation of prescription proton-pump inhibitor therapy and periodically thereafter |
|
Diuretics (i.e., loop or thiazide diuretics) |
Possible increased risk of hypomagnesemia |
Consider monitoring magnesium concentrations prior to initiation of prescription proton-pump inhibitor therapy and periodically thereafter |
|
Fosamprenavir |
Fosamprenavir: Increased esomeprazole AUC; no substantial effect on concentrations of amprenavir (active metabolite of fosamprenavir) Ritonavir-boosted fosamprenavir: No substantial effect on amprenavir or esomeprazole concentrations |
Fosamprenavir (with or without ritonavir): No dosage adjustment required |
|
Gastric pH-dependent drugs (e.g., atazanavir, digoxin, erlotinib, iron salts, ketoconazole) |
Atazanavir, erlotinib, iron salts, ketoconazole: Possible decreased absorption Digoxin: Possible increased exposure |
Digoxin: May need to monitor for manifestations of digoxin toxicity |
|
Lopinavir |
Lopinavir/ritonavir: Omeprazole had no clinically important effect on lopinavir plasma concentrations or AUC |
No dosage adjustment required when proton-pump inhibitors used with lopinavir/ritonavir |
|
Methotrexate |
Possible delayed clearance and increased serum concentrations of methotrexate and/or its metabolite hydroxymethotrexate; possible methotrexate toxicity Reported mainly with high-dose methotrexate (300 mg/m2 to 12 g/m2), but also reported with low dosages (e.g., 15 mg per week) |
Manufacturer of esomeprazole recommends considering temporary discontinuance of proton-pump inhibitor therapy in some patients receiving high-dose methotrexate Some clinicians recommend withholding the proton-pump inhibitor for several days before and after administration of either high-dose or low-dose methotrexate or, alternatively, substituting a histamine H2-receptor antagonist for the proton-pump inhibitor |
|
Nelfinavir |
Omeprazole decreased peak plasma concentrations and AUCs of nelfinavir and its major active metabolite |
Concomitant use of nelfinavir with proton-pump inhibitors not recommended |
|
NSAIAs (naproxen, rofecoxib) |
Pharmacokinetic interaction unlikely |
|
|
Oral contraceptives |
No change in esomeprazole pharmacokinetics |
|
|
Phenytoin |
Pharmacokinetic interaction unlikely |
|
|
Quinidine |
Pharmacokinetic interaction unlikely |
|
|
Raltegravir |
Omeprazole increased peak plasma concentration and AUC of raltegravir |
No dosage adjustment recommended when proton-pump inhibitors used with raltegravir |
|
Rifampin |
Possible decreased esomeprazole concentrations |
Avoid concomitant use |
|
Rilpivirine |
Omeprazole decreased plasma concentrations and AUC of rilpivirine |
Concomitant use of rilpivirine and proton-pump inhibitors contraindicated |
|
Saquinavir |
Ritonavir-boosted saquinavir: Omeprazole increased peak plasma concentration and AUC of saquinavir |
Caution advised if proton-pump inhibitor used with ritonavir-boosted saquinavir; monitor for saquinavir toxicity Manufacturer of esomeprazole recommends considering saquinavir dosage reduction on an individual basis |
|
St. John’s wort (Hypericum perforatum) |
Possible decreased esomeprazole concentrations |
Avoid concomitant use |
|
Sucralfate |
Possible delayed proton-pump inhibitor absorption and decreased bioavailability |
Administer proton-pump inhibitor at least 30 minutes before sucralfate |
|
Tacrolimus |
Possible increased tacrolimus concentrations |
|
|
Tests for neuroendocrine tumors |
Increased serum chromogranin A (CgA) concentrations (secondary to esomeprazole-induced increase in intragastric pH) may produce false-positive results |
Temporarily discontinue esomeprazole before assessing CgA concentrations and consider repeating test if initial CgA concentrations are high |
|
Voriconazole |
Possible increase in esomeprazole exposure |
Esomeprazole dosage adjustment usually not required but may be considered in patients receiving high dosages (up to 240 mg daily), such as those with Zollinger-Ellison syndrome |
|
Warfarin |
Potential for decreased warfarin metabolism and changes in prothrombin measures |
Monitor PT and INR |
Esomeprazole Pharmacokinetics
Absorption
Bioavailability
Delayed-release esomeprazole: Bioavailability is 64% after a single 40-mg oral dose. Bioavailability is 90% after repeated oral doses of 40 mg once daily.
Food
Delayed-release esomeprazole: AUC decreased by 43–53% when a 40-mg oral dose was administered with food.
Immediate-release esomeprazole/delayed-release naproxen tablets: Administration with high-fat food decreases rate and extent of esomeprazole absorption (peak plasma concentration delayed by 1 hour, AUC decreased 52%, peak concentration decreased 74%). Administration 30 minutes before high-fat food does not substantially alter rate or extent of esomeprazole absorption relative to fasted state. Administration 1 hour before high-fat food increases esomeprazole AUC and peak concentration by 25 and 50%, respectively, but peak concentration is lower than that observed with labeled dosage of esomeprazole 40 mg daily.
Special Populations
Following oral dosage of 40 mg once daily in patients with severe (Child-Pugh class C) hepatic impairment, steady-state AUCs were 2–3 times greater than those in patients with normal hepatic function.
Distribution
Extent
Not known whether esomeprazole is distributed into milk, but omeprazole is distributed into milk. Not known whether esomeprazole crosses the placenta.
Prolonged binding to gastric parietal proton pump enzyme.
Plasma Protein Binding
97%.
Elimination
Metabolism
Metabolized to inactive metabolites in the liver by CYP isoenzymes, principally by CYP2C19, and to lesser extent by CYP3A4.
Elimination Route
Excreted principally in urine (80% as inactive metabolites, <1% as active drug); remainder in feces as inactive metabolites.
Half-life
Adults, oral administration: 1–1.5 hours. Slower elimination than R-omeprazole or racemic omeprazole (0.5–1 hour).
Adults, IV administration: 1.1–1.4 hours; prolonged with increasing dose.
Adolescents 12–17 years of age, oral administration: 0.8–1.2 hours.
Children 1–11 years of age, oral administration: 0.7–0.9 hours.
Infants 1–11 months of age, oral administration: 0.9 hours.
Special Populations
In patients with poor CYP2C19 metabolizer phenotype, steady-state AUCs were 2 times greater than those in patients with extensive (or rapid) metabolizer phenotype.
Stability
Storage
Oral
Capsules
25°C (may be exposed to 15–30°C) in tightly-closed containers.
Fixed-combination Tablet (Vimovo)
25°C (may be exposed to 15–30°C) in tightly-closed containers.
Powder for Oral Suspension
25°C (may be exposed to 15–30°C).
Parenteral
Powder for IV Injection or Infusion
Powder: 25°C (may be exposed to 15–30°C). Protect from light.
Reconstituted solution: Room temperature (up to 30°C) for up to 12 hours.
Admixture: Room temperature (up to 30°C) for up to 6 hours (in 50 mL of 5% dextrose injection) or 12 hours (in 50 mL of lactated Ringer’s or 0.9% sodium chloride injection).
Compatibility
Oral
Capsules
Use extemporaneous mixture of capsule contents (enteric-coated pellets) and applesauce immediately; do not store for future use. Applesauce should not be hot.
Parenteral
Solution Compatibility34 HID
|
Compatible |
|---|
|
Dextrose 5% in water |
|
Ringer’s injection, lactated |
|
Sodium chloride 0.9% |
Drug Compatibility
|
Compatible |
|---|
|
Doripenem |
Actions
-
Inhibits basal and stimulated gastric acid secretion.
-
Concentrates in acid conditions of parietal cell secretory canaliculi; forms active sulfonamide metabolite that irreversibly binds to and inactivates hydrogen-potassium ATPase (proton- or acid pump), blocking final step in secretion of hydrochloric acid. Acid secretion is inhibited until additional hydrogen-potassium ATPase is synthesized, resulting in prolonged duration of action.
-
More esomeprazole reaches and blocks proton pump than does R-omeprazole; therefore, provides greater intragastric pH control than racemic omeprazole.
-
Suppresses H. pylori in patients with duodenal ulcer and/or reflux esophagitis who are infected with the organism. Combined therapy with esomeprazole and appropriate anti-infectives (i.e., amoxicillin, clarithromycin) can effectively eradicate H. pylori gastric infection.
Advice to Patients
-
Importance of swallowing capsule intact, without crushing or chewing.
-
Importance of taking 1 hour before a meal.
-
If capsule contents are mixed with applesauce for administration, importance of applesauce being soft enough to swallow without chewing. Importance of not using hot applesauce. Importance of immediately swallowing mixture without crushing or chewing; do not store for later use.
-
If oral suspension is used, importance of mixing packet contents with an appropriate amount of water, allowing mixture to thicken for 2–3 minutes, and then drinking mixture (without crushing or chewing the granules) within 30 minutes of preparation.
-
Importance of advising patients that use of multiple daily doses of the drug for an extended period of time may increase the risk of fractures of the hip, wrist, or spine.
-
Risk of hypomagnesemia; importance of immediately reporting and seeking care for any cardiovascular or neurologic manifestations (e.g., palpitations, dizziness, seizures, tetany).
-
Possible increased risk of Clostridium difficile infection; importance of contacting a clinician if persistent watery stools, abdominal pain, and fever occur.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs. Antacids may be used concomitantly as needed for pain relief.
-
Importance of women informing their clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules, delayed-release (containing enteric-coated pellets) |
20 mg (of esomeprazole) |
NexIUM |
AstraZeneca |
|
40 mg (of esomeprazole) |
NexIUM |
AstraZeneca |
||
|
For suspension, delayed-release (containing enteric-coated granules) |
2.5 mg (of esomeprazole) per packet |
NexIUM |
AstraZeneca |
|
|
5 mg (of esomeprazole) per packet |
NexIUM |
AstraZeneca |
||
|
10 mg (of esomeprazole) per packet |
NexIUM |
AstraZeneca |
||
|
20 mg (of esomeprazole) per packet |
NexIUM |
AstraZeneca |
||
|
40 mg (of esomeprazole) per packet |
NexIUM |
AstraZeneca |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, delayed-release core (naproxen only) |
20 mg (of esomeprazole) with Naproxen 375 mg |
Vimovo |
AstraZeneca |
|
20 mg (of esomeprazole) with Naproxen 500 mg |
Vimovo |
AstraZeneca |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
For injection, for IV use |
20 mg (of esomeprazole) |
NexIUM I.V. |
AstraZeneca |
|
40 mg (of esomeprazole) |
NexIUM I.V. |
AstraZeneca |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions January 31, 2013. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Frequently asked questions
More about esomeprazole
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (273)
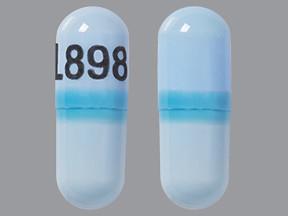
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: proton pump inhibitors
- Breastfeeding
Patient resources
Professional resources
- Esomeprazole prescribing information
- Esomeprazole Capsules (FDA)
- Esomeprazole Injection (FDA)
- Esomeprazole Oral Suspension (FDA)
- Esomeprazole Strontium Capsules (FDA)